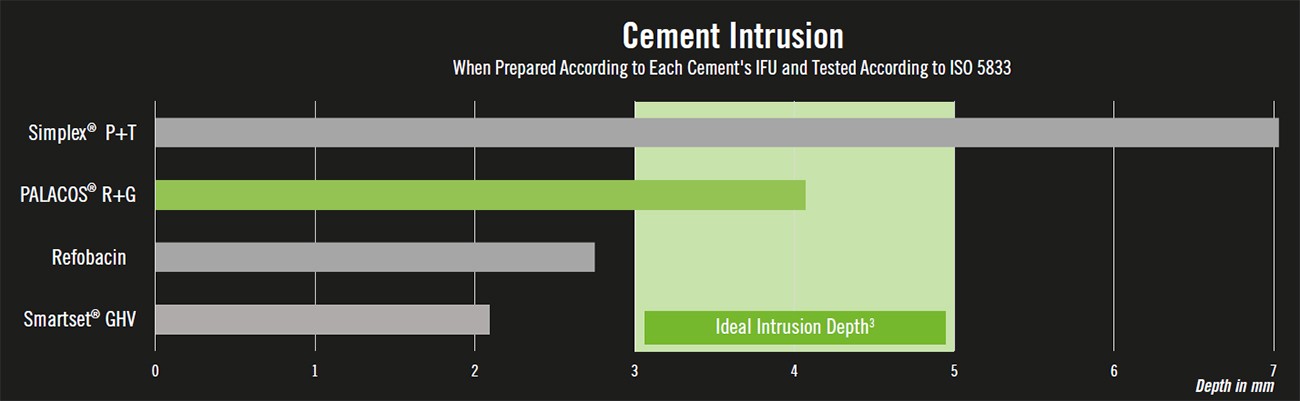
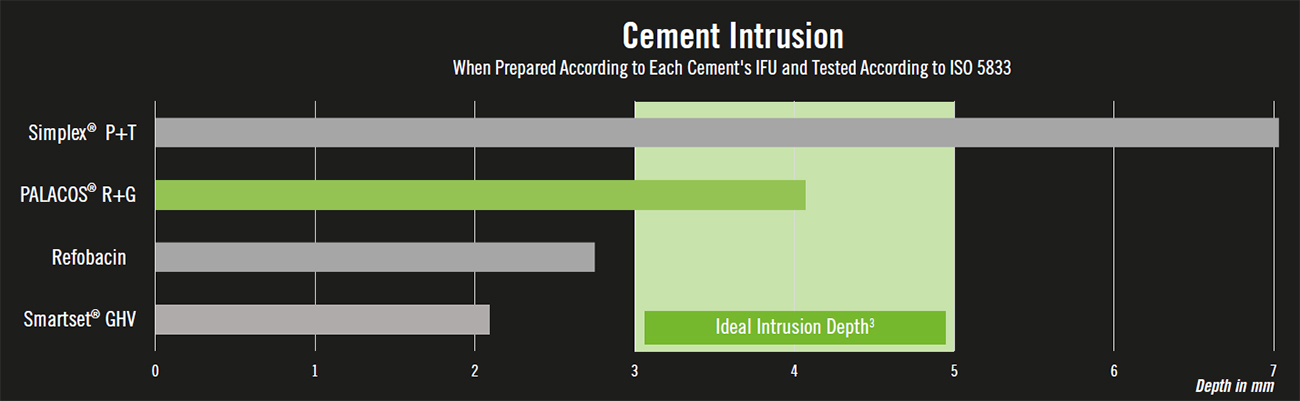
In a 2011 study, Jan Vanlommel and colleagues reviewed the literature related to cement interdigitation in TKA and declared that 3 to 5 mm of cement penetration was ideal in providing excellent implant stability.3 Building on this study, it has been found that improperly intruded cement can cause many complications. Too high, and the risk of thermal necrosis4 and BCIS5 increase; too low, and the cement-bone interface provides more reduced shear strength, as well as a higher risk of aseptic loosening and revision over time.6 High intrusion also reduces the amount of bone stock remaining in the event of revision.7 Importantly, the high intrusion of Simplex P+T® in the above study was also observed in a study conducted by Stryker employees.8
For additional resources on this study, see the
bottom of this page
.
PALACOS® At The Cement-Bone Interface
After sixty years of experience as the inventor and sole manufacturer of PALACOS®-the gold standard in joint fixation1-Heraeus Medical has transitioned to be the exclusive provider for the PALACOS® cements family in the U.S (PALACOS® R/R+G, PALACOS® MV/MV+G, PALACOS® LV/LV+G, PALACOS® R/R+G pro). Characteristically green in color, PALACOS® doesn’t just claim to be the element of success in joint replacement, it continuously proves it as the most studied bone cement worldwide.2
Achieve Ideal Intrusion With PALACOS®
Application Matters

The use of a cement gun enables higher pressurization of cement during application to the tibial plateau and aids in interdigitation into cancellous bone.
The PALAMIX® Cement Gun from Heraeus Medical has won an international design award9 for its ease of use and is compatible with the PALAMIX® and PALACOS® R pro vacuum mixing systems.
Consistency is Key

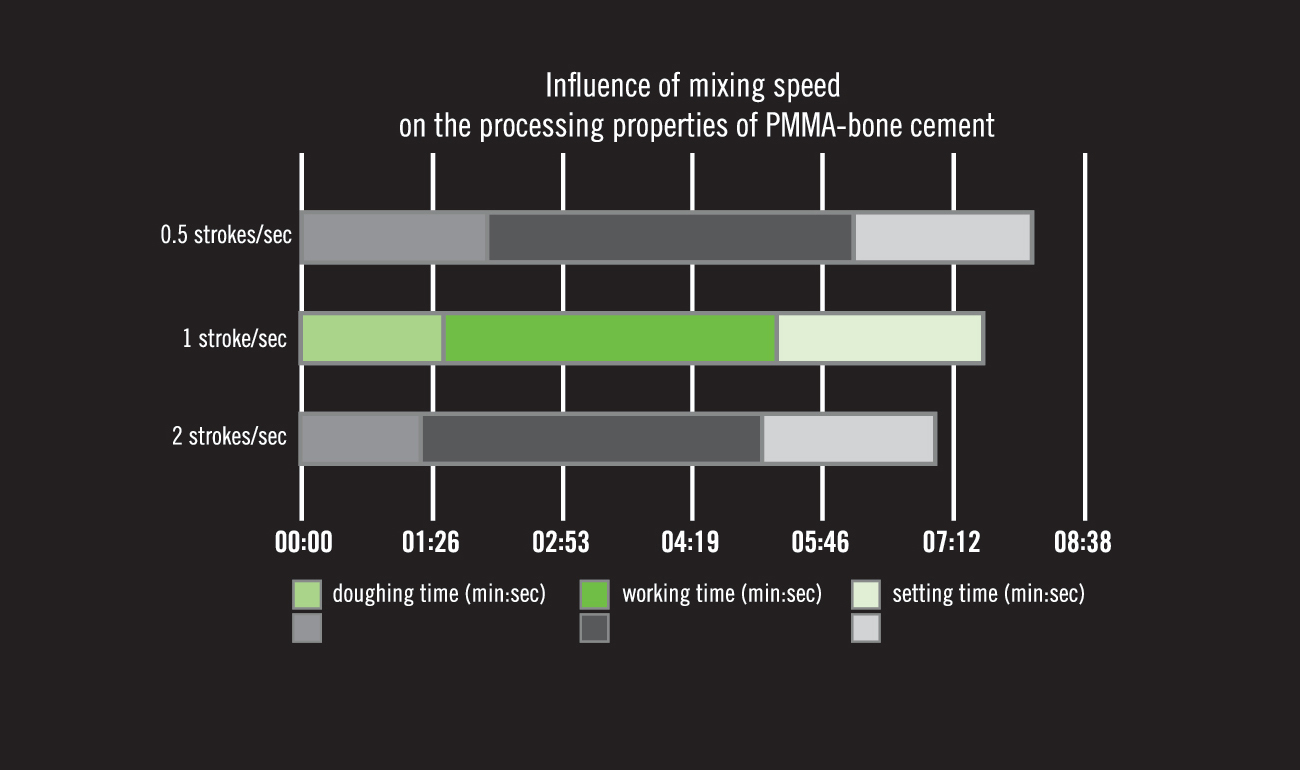
In addition to temperature, humidity, and use of vacuum, the polymerization reaction of all bone cements changes based on the speed of operator mixing. Based on our research and experience, we recommend mixing PALACOS® R at one stroke per second.
The use of power mixing devices that drastically increase the speed of mixing is likely to impact the polymerization reaction and may lead to the premature setting of the cement. The accidental movement of the implant when the cement has prematurely moved into the setting phase will lead to debonding at the cement-implant interface.
Because of this, we do not recommend the use of power vacuum mixing devices when preparing PALACOS® R.
Optimize Cement-Implant Strength with PALACOS®
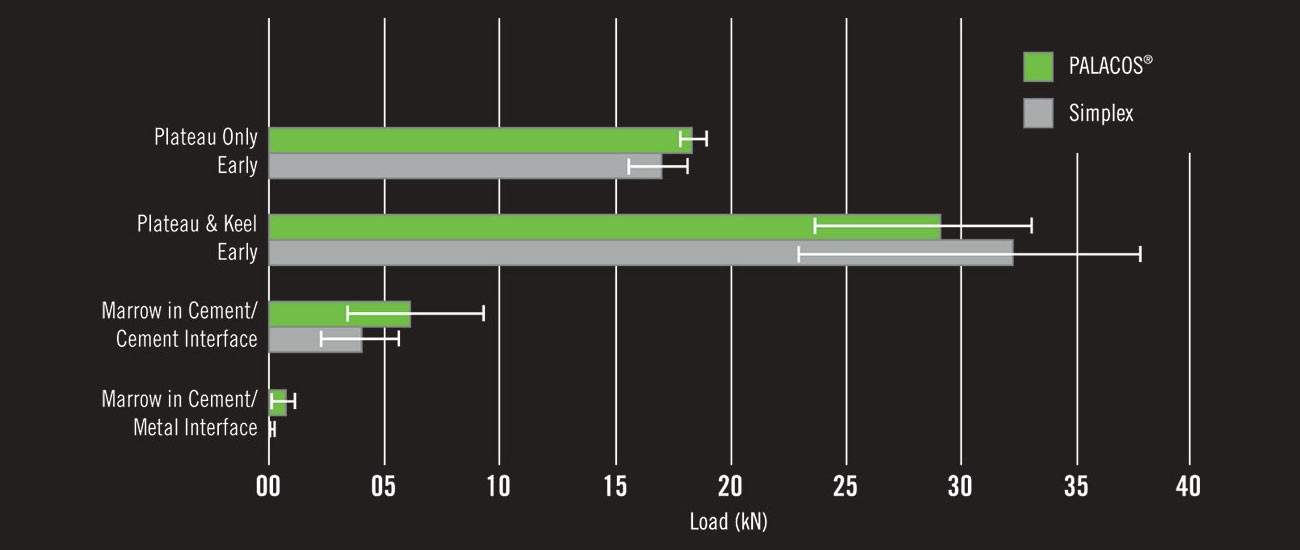
Application of cement to body tissues when still in the waiting (or sticky) phase is contraindicated as it increases the risk of bone cement implantation syndrome (BCIS). However, early application of the cement to the metal surface of the implant ex vivo appears to strengthen the cement-implant bond. PALACOS® R performs especially well during this early phase and when contamination is present.10
Literature:
1 Olerud et.al.: Comparison of Refobacin Bone Cement and Palacos with Gentamicin in total hip arthroplasty; an RSA study with two years follow-up, Hip int., 2013:1.
2 Pilz V, Hanstein T. A literature review of the clinical evidence of bone cements. RRJMHS 2018; 7(1): 31-36.
3 Vanlommel J, et al. Cementing the TIbial Component in Total Knee Arthroplasty: Which Technique is the Best? J Arthroplasty 2011; 26(3): 492-496.
4 Huiskes R, Sloof TJ. Thermal injury of cancellous bone following pressurized penetration of acrylic bone cement. Proc 27th Orthop Res Soc, Las Vegas; 1981; p 134.
5 Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Aneasth 2009; 102(1): 12-22.
6 Kuhn KD. PMMA Cements. Noval Comparative Data (Table 13.2). Berlin: Springer; 2014.
7 Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award Paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res 2002; 404: 7-13.
8 He S, Sagato F, Klein R, Mulvihill H, Bogatch Y. Comparative Handling, Intrustion and Antibiotic Elution Characteristics of Simplex HV Bone Cement. ORS 2014 Annual Meeting. Poster 1849.
9 Gerber E. Design Preis Scheweiz 99. Zürich: Hochparterre; 1999: 14-15.
10 Billi F, Kavanaugh A, Schmalzried TP. Techniques for improving the initial strength of the tibial tray-cement interface bone. Bone Joint J 2019; 101-B (1 Supple A): 53-8.
Figures:
Figure 1: Kuehn KD. PMMA Cements. Novel Comparative Data (Table 13.2). Berlin: Springer, 2014.
Figure 2: Lutz MJ, Pincus PF, Whitehouse SL, Halliday BR. The Effect of Cement Gun and Cement Syringe Use on Tibial Cement Mantle in Total Knee Arthroplasty. J Arthoplasty 2009; 24(3): 461-7.
Figure 3: Sigmund IK, Gamper J, Antoni A, et al. Mixing Technique of PMMA: Bone Cement Determines the Ideal Insertion Time Point in Cement Joint Arthroplasty. J Surg 2018; 12: 1-8.
Figure 4: Billi F, Kavanaugh A, Schmalzried TP. Techniques for improving the initial strength of the tibial tray-cement interface bone. Bone Joint J 2019; 101-B (1 Supple A): 53-8.
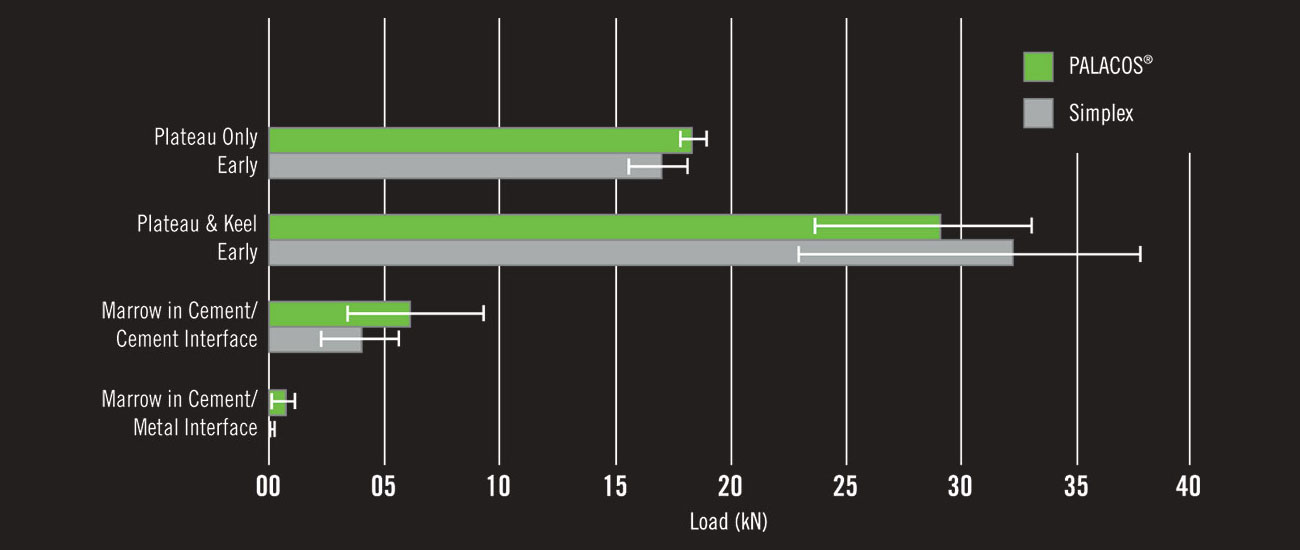
Klaus Dieter Kuehn and colleagues at the University of Gratz determined the intrusion of various antibiotic loaded bone cements when prepared according to the manufacturer’s IFU at 23 degrees Celsius and in humidity >40%.1 The specific methodology for determining interdigitation followed International Standards for testing bone cement (ISO 5833). Importantly, the high intrusion of Simplex P+T in this study was also observed in a study conducted by Stryker employees.2
In an oft-cited 2011 Journal of Arthroplasty article, Jan Vanlommel and colleagues reviewed the literature related to cement interdigitation in TKA and declared that 3 to 5 mm of cement penetration was ideal.3 Vanlommel based the minimum interdigitation requirement on several in vitro studies which found that with 3 mm of cement mantle underneath the tibial tray, the cement crossed at least one level of transverse trabeculae and led to excellent stability of the implant.
The maximum recommended interdigitation is based on several studies which have found increased adverse events with greater cement mantles.
- Rik Huiskes initially described the linear relationship between interdigitation and risk of thermal injury in total joint replacement.4 More recently, M.R. Whitehouse and colleagues from the University of Bristol exposed femoral neck bone from patients undergoing THA to either 5 or 7 mm of cement interdigitation.5 The investigators monitored the surface and core temperature of the bone and determined the percent of osteocytes still viable after the bone cement had fully cured. At 5 mm of intrusion, in vivo bone spent 11 seconds above 55 degrees Celsius and no time above 70 degrees Celsius. In contrast, in vivo bone exposed to 7 mm of intrusion spent 33 seconds above 55 degrees Celsius and 11 seconds above 70 degrees Celsius. Temperatures greater than 55 degrees Celsius result in marrow necrosis while temperatures in excess of 70 degrees Celsius result in macroscopic bone necrosis. On LDH assay, 37.9% (95% CI: 32.2 to 41.2%) of the osteocytes from the femoral head with 5 mm of intrusion remained viable versus 24.5% (95% CI: 17.7 to 52.3%) of osteocytes from the bone exposed to 7 mm of intrusion.
- Bone cement implantation syndrome results from increased intramedullary pressures forcing fat, marrow and other contents through the cancellous bone and into the vasculature.6 Increased interdigitation decreases the distance between the vasculature and material of embolic potential. The increased risk of BCIS with higher intrusion is supported by findings from the Mayo Clinic Registry. In a review of patients experiencing sudden cardiac collapse due to bone cement implantation syndrome during THA between 1969 and 1997, three of 13 patients (23%) had methylmethacrylate particles embolized in their lungs. This suggests that bone cement expansion into the cancellous bone is forcing other particles (and sometimes bone cement itself) into particles are passing out of bone and into circulation. Further, the authors of the Mayo Registry study speculated that patients with osteoporosis were at greater risk of BCIS because the increased porosity of their bone enabled embolic material to more easily pass into their circulation.7
References
1 Kuehn KD. PMMA Cements. Novel Comparative Data (Table 13.2). Berlin: Springer, 2014.
2 He S, Sagato F, Klein R, Mulvihill H, Bogatch Y. Comparative Handling, Intrusion and Antibiotic Elution Characteristics of Simplex HV Bone Cement. ORS 2014 Annual Meeting. Poster 1849.
3 Vanlommel J, et al. Cementing the TIbial Component in Total Knee Arthroplasty: Which Technique is the Best? J Arthroplasty 2011; 26(3): 492-496.
4 Huiskes R. Some fundamental aspects of human joint replacement. Analyses of stresses and heat conduction in bone-prosthesis structures. Acta Orthop. Scand. Suppl. 1980; 185:1–208 Whitehouse MR, Atwal NS, Pabbruwe M, Bloom AW, Bannister GC. Osteonecrosis with tuse of Polymethylmethecrylate Cement for Hip Replacement: Thermal-Induced Damage Evidenced In Vivo by Decreased Osteocyte Viability. Eur Cells Mater 2014; 27: 50-63.
5 Donaldson AJ, Thomson HE, Harper NJ, Kenny MW. Bone Cement Implantation Syndrome. Br J Anaesth 2009; 102(1): 12-22.
6 Parvizi J, Holliday AD, Ereth MH, Lewallen DG. Sudden Death during Primary Hip Arthroplasty. CORR 1999; 369: 39-48.